नए एंटीबायोटिक टीक्सोबैक्टीन की खोज
नए एंटीबायोटिक टीक्सोबैक्टीन की खोज
टीक्सोबैक्टीन नाम के नए एंटीबायोटिक की खोज मैसाचुसेट्स के बोस्टन में नॉर्थइस्टर्न यूनिवर्सिटी के वैज्ञानिकों की टीम ने की. करीब तीन दशकों के बाद पहली बार खोजा गया यह एंटीबायोटिक ऐसे संक्रमणों से लड़ने में सक्षम है जो हर वर्ष सैंकड़ों – हजारों लोगों की मौत की वजह बनते हैं.
यह खोज 7 जनवरी 2005 को नेचर नाम के जनरल में ऑनलाइन प्रकाशित हुआ था.
टेक्सोबैक्टीन के गुण
• टेक्सोबैक्टीन लिपिड II ( पेप्टीडोग्लायकन के अग्रदूत) और लिपिड III ( कोशिका दीवार टीकोइक एसिड के अग्रदूत ) के अत्यधिक संरक्षित मूल भाव को बांध कर दीवार संश्लेषण को रोकता है.
• स्टाफिलोकोक्कस ऑरियस या माइकोबैक्टेरियम ट्यूबरकुलोसिस प्रतिरोधी का कोई भी म्यूटेंट टेक्सोबैक्टीन से प्राप्त किया जा सकता है.
• इस यौगिक के गुण ऐसे एंटीबायोटिक्स को विकसित करने का रास्ता बताते हैं जो प्रतिरोध क्षमता को कम करता है.
टेक्सोबैक्टीन की प्राप्ति ?
टेक्सोबैक्टीन एंटीबोटिक को असंवर्धित बैक्टीरिया से सीटू की खेती या विशेष विकास कारकों का प्रयोग कर प्राप्त किया गया है. इसके लिए असंवर्धित बैक्टीरिया का प्रयोग इसलिए किया गया क्योंकि टीम का मानना था कि बाहरी वातावरण में मौजूद सभी प्रजातियों में से लगभग 99 फीसदी नए एंटीबायोटिक दवाओं के अप्रयुक्त स्रोत हैं.
यह खोज आवश्यक क्यों है?
पहला एंटीबायोटिक पेनिसिलिन की खोज 1928में एलेक्जेंडर फ्लेमिंग ने की थी औऱ तब से 100से अधिक यौगिकों की खोज हो चुकी है. एंटीबायोटिक्स की खोज के महत्वपूर्ण दशक 1950 और 1960 के दशक थे लेकिन 1987 के बाद से कोई भी नया श्रेणी नहीं मिला था.
नए एंटीबायोटिक या दवा की जरूरत इसलिए महत्वपूर्ण है क्योंकि मलेरिया और एमडीआर टीबी (क्षयरोग) अब लाइलाज बन गए हैं क्योंकि इन बीमारियों ने वर्तमान में मौजूद एंटीबायोटिक की श्रेणी के खिलाफ प्रतिरोध क्षमता विकसित कर ली है, जिसकी वजह से सार्वजनिक स्वास्थ्य समस्या पैदा हो गई है. यह खोज दवाओं के प्रति बढ़ते प्रतिरोध क्षमता से लड़ने में फायदेमंद हो सकता है.
———————————————————————————————–
What are antibiotics?
The US National Library of Medicine1 says that antibiotics – powerful medicines that fight bacterial infections – can save lives when used properly. Antibiotics either stop bacteria from reproducing or kill them. “Your body’s natural defenses can usually take it from there.”
Before bacteria can multiply and cause symptoms, the body’s immune system can usually destroy them. We have special white blood cells that attack harmful bacteria. Even if symptoms do occur, our immune system can usually cope and fight off the infection. There are occasions, however, when it is all too much and some help is needed…..from antibiotics.
The first antibiotic was penicillin. Such penicillin-related antibiotics as ampicillin, amoxicillin and benzylpenicilllin are widely used today to treat a variety of infections – these antibiotics have been around for a long time.
There are several different types of modern antibiotics and they are only available with a doctor’s prescription in most countries.
Overusing antibiotics – There is concern worldwide that antibiotics are being overused. Antibiotic overuse is one of the factors that contributes towards the growing number of bacterial infections which are becoming resistant to antibacterial medications.
According to the CDC (Centers for Disease Control and Prevention), outpatient antibiotic overuse in the USA is a particular problem in the Southeast.
The ECDC (European Centre for Disease Prevention and Control) says that antibiotic resistance continues to be a serious public health threat worldwide. In a statement issued in 19th November 2012, the ECDC informed that an estimated 25,000 people die each year in the European Union from antibiotic-resistant bacterial infections.
New ECDC data has shown that there has been a considerable increase over the last four years of combined resistance to multiple antibiotics in E. coli and Klebsiella pneumoniae in over one third of EU and EEA (European Economic Area) nations. Consumption of carbapenems, a major class of last-line antibiotics, increased significantly from 2007 to 2010.
Antibiotic resistance: how has it become a global threat to public health? Then there is the danger that the ignorant man may easily underdose himself and by exposing his microbes to non-lethal quantities of the drug, make them resistant,” said Alexander Fleming, speaking in his Nobel Prize acceptance speech in 1945. As predicted almost 70 years ago by the man who discovered the first antibiotic, drug resistance is upon us.
How do antibiotics work?
Although there are a number of different types of antibiotic they all work in one of two ways:
- A bactericidal antibiotic kills the bacteria. Penicillin is a bactericidal. A bactericidal usually either interferes with the formation of the bacterium’s cell wall or its cell contents.
- A bacteriostatic stops bacteria from multiplying.
What are antibiotics for?
An antibiotic is given for the treatment of an infection caused by bacteria. Antibiotics target microorganisms such as bacteria, fungi and parasites. However, they are not effective against viruses.
If you have an infection it is important to know whether it is caused by bacteria or a virus. Most upper respiratory tract infections, such as the common cold and sore throats are generally caused by viruses – antibiotics do not work against these viruses.
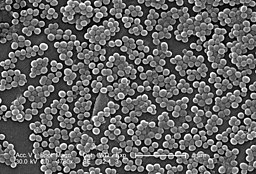
Electron micrograph of clumps of methicillin-resistant Staphylococcus aureus (MRSA) bacteria, which are becoming more resistant to antibiotics.
If antibiotics are overused or used incorrectly there is a risk that the bacteria will become resistant – the antibiotic becomes less effective against that type of bacterium.
A broad-spectrum antibiotic can be used to treat a wide range of infections. A narrow-spectrum antibiotic is only effective against a few types of bacteria. There are antibiotics that attack aerobic bacteria, while others work against anaerobic bacteria. Aerobic bacteria need oxygen, while anaerobic bacteria don’t.
Antibiotics may be given beforehand, to prevent infection, as might be the case before surgery. This is called ‘prophylactic’ use of antibiotics. They are commonly used before bowel and orthopedic surgery.
What are the side-effects of antibiotics?
Below is a list of the most common side-effects of antibiotics:
- Diarrhea – researchers from Stanford University School of Medicine found that a rise in sugars in the gut following antibiotic treatment allows harmful bacteria to get a foothold and cause infection. Harmful bacteria thrive on sugar.
- Feeling and being sick.
- Fungal infections of the mouth, digestive tract and vagina.
Below is a list of rare side-effects of antibiotics:
- Formation of kidney stones (when taking sulphonamides).
- Abnormal blood clotting (when taking some cephalosporins).
- Sensitivity to sun (when taking tetracyclines).
- Blood disorders (when taking trimethoprim).
- Deafness (when taking erythromycin and the aminoglycosides).
Some patients, especially elderly ones, may experience inflamed bowels (a type of colitis) which can lead to severe diarrhea. Clindamycin, an antibiotic used for the most serious infections, commonly has this side effect. However, although much less common, penicillins, cephalosporins and erythromycin might do too.
In August 2012, Scientists from the NY School of Medicine found that babies who are exposed to antibiotics have a greater risk of becoming overweight or obese children. Their study was published in the International Journal of Obesity.
Allergic reactions to antibiotics
Some patients may develop an allergic reaction to antibiotics – especially penicillins. Side effects might include a rash, swelling of the tongue and face, and difficulty breathing.
Allergic reactions to antibiotics may be immediate or delayed hypersensitivity reactions2.
If you have ever had an allergic reaction to an antibiotic you must tell your doctor and/or pharmacist. Reactions to antibiotics can be very serious, and sometimes fatal – they are called anaphylactic reactions.
Use antibiotics with extreme caution and ensure you inform your doctor/pharmacist if:
- You have reduced liver or kidney function.
- You are pregnant
- You are breastfeeding
Antibiotics may clash (interact) with other medicines
If you are taking an antibiotic do not take other medicines or herbal remedies without telling your doctor first. OTC (over the counter, non-prescription) medicines might also clash with your antibiotic.
Penicillins, cephalosporins, and some other antibiotics may undermine the effectiveness of oral contraceptives. If the antibiotic has caused diarrhea/vomiting the absorption of contraceptives may also be disrupted. If you are taking any of these drugs you should consider taking additional contraceptive precautions.
How to use antibiotics
Antibiotics are usually taken by mouth (orally); however, they can also be administered by injection, or applied directly to the affected part of the body.
Most antibiotics start having an effect on an infection within a few hours. It is important to remember to complete the whole course of the medication to prevent the infection from coming back.
If you do not complete the course, there is a higher chance the bacteria may become resistant to future treatments – because the ones that survive when you did not complete the course have had some exposure to the antibiotic and may consequently have built up a resistance to it. Even if you are feeling better, you still need to complete the course.
Some antibiotics should not be consumed with certain foods and drinks. Others should not be taken with food in your stomach – these would normally be taken about an hour before meals, or two hours after. It is crucial that you follow the instructions correctly if you want the medication to be effective. If you are taking metronidazole do not consume alcohol.
Dairy products should not be consumed if you are taking tetracyclines, as they might affect the absorption of the medication.






 +91-94068 22273
+91-94068 22273 
